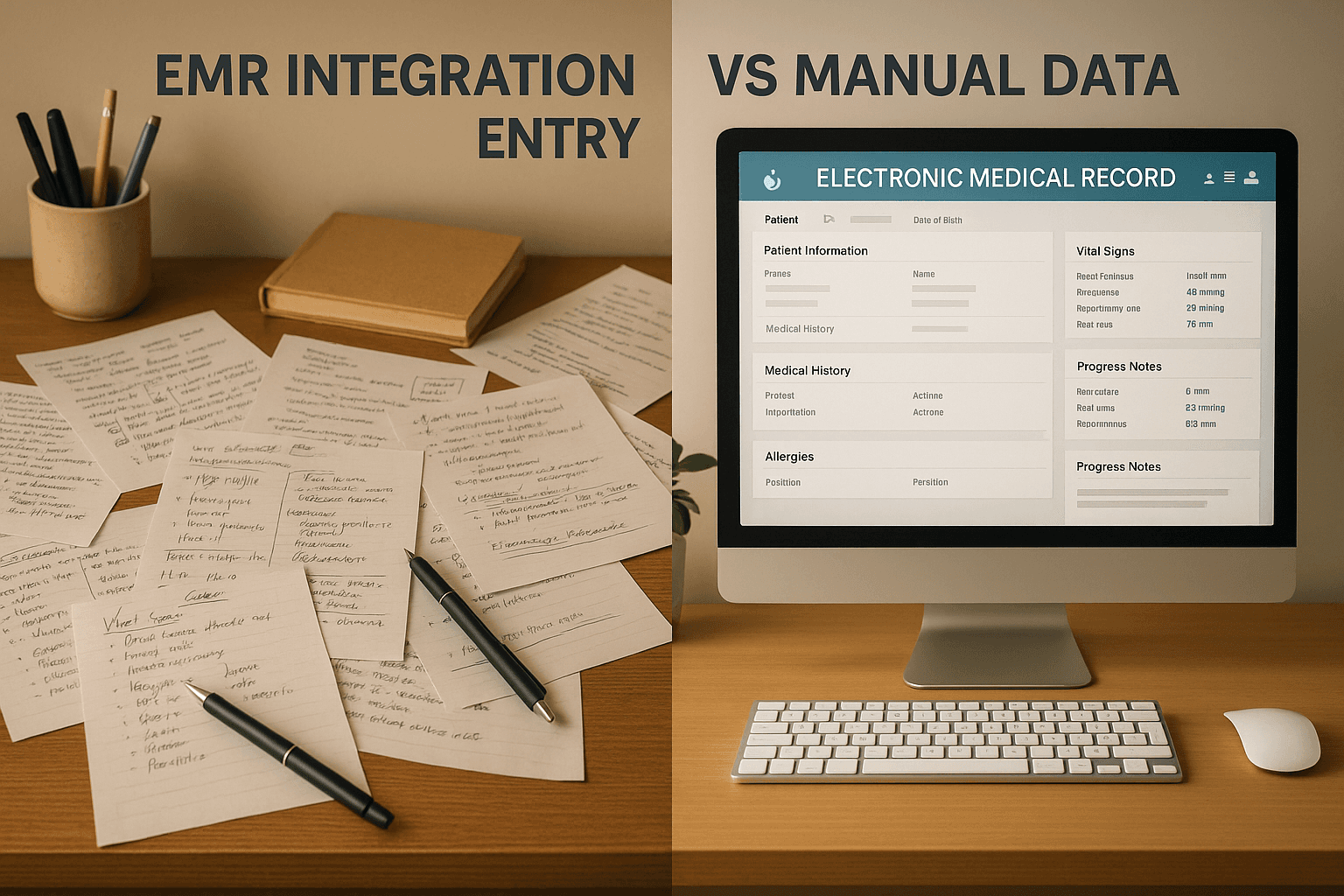
EMR Integration vs Manual Data Entry: Which Wins?
Nov 24, 2025
EMR Integration vs Manual Data Entry: Which Wins?
EMR integration is the clear winner over manual data entry. Here’s why:
Efficiency: EMR integration automates repetitive tasks like data sharing, saving time and reducing administrative burdens.
Accuracy: Automation minimizes errors, ensuring critical details like medications and allergies are always correct.
Compliance: Integrated systems meet HIPAA standards with automated audit trails, reducing the risk of data breaches.
Scalability: EMR systems handle growing patient volumes without requiring more staff.
Patient Care: Less time on manual tasks means more focus on patients, shorter wait times, and faster decision-making.
Manual data entry, by contrast, is slow, error-prone, and labor-intensive. It increases risks, administrative costs, and staff burnout, ultimately affecting patient outcomes.
Quick Comparison
Factor | EMR Integration | Manual Data Entry |
|---|---|---|
Time Efficiency | Automates data sharing, saving hours daily | Slows operations with repetitive tasks |
Error Rates | Low due to automation | High due to human mistakes |
Compliance | Built-in HIPAA compliance | Relies on manual tracking |
Scalability | Handles growth without extra staff | Requires more staff as patient load grows |
Patient Care | Improves focus on care | Reduces time available for patients |
Switching to EMR integration is a smart move for clinics aiming to improve operations, reduce costs, and deliver better care.
Here’s How EHR Integration Is A Game-Changer for Hospital Efficiency and Quality Care! #healthtech
How EMR Integration Improves Clinic Workflows
Integrated EMR systems streamline clinic operations by ensuring smooth data communication and removing manual inefficiencies.
Automation and Workflow Efficiency
One major advantage of EMR integration is cutting down on repetitive tasks that often eat up valuable staff hours. For instance, instead of manually transcribing lab results from faxes into patient charts, integrated systems automatically update key information across all necessary platforms.
These systems can handle tasks like auto-populating patient data, sending electronic referrals, and sorting incoming documents. Tools like Diagna's FAXFlo use AI to manage these processes, saving time and reducing the need for manual tracking. Over a typical workday, these efficiencies free up staff to concentrate more on patient care. Plus, these streamlined workflows contribute to much higher levels of data accuracy.
Accuracy and Error Reduction
With EMR integration, data only needs to be entered once, and it updates across all connected systems. This helps protect critical details such as medication dosages and allergy information. For example, when lab results are uploaded directly into an EMR, the chances of errors from misreading handwritten notes or typos are almost entirely removed. Similarly, when pharmacy systems sync with EMRs, medication reconciliation becomes more reliable, reducing the risk of harmful drug interactions.
Better data accuracy doesn’t just enhance patient safety - it also minimizes financial losses from billing mistakes. Features like automated coding suggestions and instant insurance eligibility checks make billing and claims processing more dependable.
Prior authorization also benefits from these improvements. Automated tools like Diagna's Prior Auth Bot pull accurate patient information directly from EMR records, ensuring forms are complete and submitted with the right insurance details. This streamlines the approval process while improving compliance and interoperability.
Compliance and Interoperability
Integrated EMR systems help maintain HIPAA compliance by automatically logging every instance of data access or modification, eliminating the gaps that often come with manual documentation.
Standards like HL7 and FHIR enable secure and efficient data sharing between different healthcare systems. This ensures that when patients move between providers, their essential clinical information transfers automatically, reducing risks like data loss or privacy breaches.
Additionally, integrated systems simplify quality reporting for programs like Medicare and Medicaid by capturing and organizing data on patient outcomes and care coordination. By automating compliance tracking and data sharing, EMRs allow clinical teams to focus more on providing excellent patient care instead of being bogged down by administrative tasks.
Problems with Manual Data Entry
Even with the clear advantages of EMR integration, manual data entry remains a persistent challenge for healthcare practices in the United States. These issues disrupt workflows and can negatively affect patient care, emphasizing the need for integrated systems in modern healthcare.
High Administrative Burden
Manual data entry slows down routine clinical operations significantly. Staff often spend countless hours transferring information from paper forms, faxes, and phone calls into various systems. The workload becomes even heavier when the same data needs to be entered into multiple platforms. During busy periods, this can lead to overtime as staff race to keep up with repetitive tasks. This time-consuming process stands in stark contrast to the streamlined efficiency of EMR integration.
Increased Risk of Errors
Manual data entry is prone to errors that can have serious consequences. Mistakes like swapped patient IDs, incorrect medication dosages, or misspelled names can lead to billing problems, delayed referrals, or even compromised patient safety. Handwritten notes add another layer of risk, as they are often misread or misinterpreted. Fixing these errors takes additional time and effort, compounding the administrative workload. In comparison, EMR integration offers a far more reliable and accurate alternative.
Strain on Patient Care
The inefficiencies of manual data entry ultimately take time away from patient care. When staff are bogged down with data entry tasks, they have less availability for patient-focused activities like answering questions, providing education, or assisting with clinical procedures. This can lead to longer wait times, delays in returning calls, and scheduling complications. Moreover, these inefficiencies can slow down clinical decision-making and contribute to provider burnout, further reducing the quality of care patients receive. All of this highlights the stark difference between manual processes and the streamlined precision of EMR integration.
EMR Integration vs Manual Data Entry: Side-by-Side Comparison
Looking at these two approaches side by side highlights their operational differences. This comparison can help clinic administrators decide which strategy better supports efficient workflows and high-quality patient care.
Comparison Table
Here’s a breakdown of how EMR integration stacks up against manual data entry in key operational areas:
Factor | EMR Integration | Manual Data Entry |
|---|---|---|
Time Efficiency | Automated data transfer speeds up processing significantly. | Requires considerable time daily for repetitive tasks. |
Error Rates | Automated validation reduces the likelihood of errors. | Prone to human mistakes and misinterpretation. |
Staff Productivity | Frees up staff to focus more on patient care. | Ties up staff with time-consuming administrative tasks. |
Compliance | Includes built-in HIPAA compliance and automated audit trails. | Relies on manual tracking, making compliance more complex. |
Scalability | Easily handles increased patient loads without extra staffing. | Requires additional staff as patient volumes grow. |
Initial Investment | Requires upfront costs but offers long-term savings through efficiency. | Lower initial costs but higher ongoing operational expenses. |
Data Accessibility | Enables real-time access across systems and locations. | Limited to physical locations and standard business hours. |
Patient Satisfaction | Leads to faster service and shorter wait times. | Can result in delays and longer processing times. |
This table makes it clear: automation offers a major edge in efficiency and cost-effectiveness compared to manual methods.
While EMR integration requires an initial investment, its long-term benefits - like reduced labor costs and smoother compliance - often justify the expense. It also helps clinics manage peak periods without disruptions, avoiding the bottlenecks that manual processes often face during busy times. Although there may be a learning curve when implementing a new system, the payoff includes fewer repetitive tasks and more time for patient care. On the other hand, manual data entry demands constant vigilance, with higher risks of errors and ongoing quality control efforts to keep operations running smoothly.
Examples of Successful EMR Integration
When it comes to electronic medical record (EMR) integration, real-world examples show just how transformative these systems can be. Across the U.S., healthcare facilities are leveraging automation tools to simplify workflows and improve patient care.
Case Studies of EMR Success
Streamlining Fax Management with AI
A multi-specialty clinic in California faced a major hurdle: an overwhelming number of faxes that slowed down the identification of urgent information. Enter Diagna's FAXFlo system. This AI-driven tool categorizes and routes faxes based on their type and urgency. The result? Faster document processing, more time for staff to focus on patients, and critical lab results reaching doctors without delay.
Cutting Patient Wait Times with Automated Referral Tracking
In Texas, a primary care practice struggled with manual referral tracking, leading to communication breakdowns and delays. By adopting Diagna's Referral Manager, the practice introduced real-time tracking for referrals, ensured timely follow-ups, and drastically reduced patient wait times. This not only improved patient care but also lightened the administrative workload for staff.
Speeding Up Prior Authorizations
A cardiology practice in Florida was bogged down by delays in insurance prior authorizations due to manual processing. After implementing Diagna's Prior Auth Bot, the practice automated the creation and electronic submission of forms. This change slashed processing times, enabling patients to receive treatments sooner while boosting administrative efficiency.
Lessons Learned from EMR Implementation
Practical experiences reveal several important takeaways for ensuring smooth and effective EMR integration.
Start with Simple, High-Impact Processes
Kick off your EMR integration journey with administrative tasks that are straightforward yet deliver immediate results. For instance, focus on automating document management or referral tracking. These "quick wins" not only improve efficiency but also help staff see the value of automation early on, building support for larger initiatives.
Ensure Compatibility with Existing Systems
Choose solutions that work seamlessly with your current EMR setup, avoiding the need for extensive data migrations or system overhauls. For example, Diagna's platform integrates with both modern and legacy systems, allowing clinics to enhance their operations without disrupting existing workflows.
Keep It User-Friendly
The best automation tools simplify routines rather than complicate them. Opt for platforms with intuitive, web-based interfaces that require minimal training. Whether in the office or working remotely, staff should be able to manage workflows effortlessly, addressing common productivity challenges tied to manual data entry.
Make HIPAA Compliance a Priority
From day one, ensure that your automation tools meet healthcare privacy standards. Features like built-in compliance protocols, detailed audit trails, and secure data handling protect patient confidentiality and prevent costly violations, fostering trust during the transition to digital systems.
Track Results and Adapt
Monitor key metrics such as processing times, error rates, staff productivity, and patient satisfaction before and after implementation. Regularly reviewing these indicators allows practices to fine-tune their systems, maximizing efficiency and demonstrating the clear advantages of automation over manual processes.
Which Wins?
When it comes to modern healthcare practices, the verdict is clear: EMR integration leaves manual data entry far behind.
Key Takeaways
The comparison between these two approaches highlights major differences in efficiency and outcomes:
Automation: EMR integration streamlines tasks, slashes processing times, and minimizes errors.
Accuracy: Automated systems ensure consistent data quality, whereas manual processes often lead to costly mistakes.
Financial Benefits: Lower administrative overhead speeds up revenue cycles and improves cash flow.
Scalability: As practices grow, manual methods demand more staff, while EMR systems scale effortlessly without proportional staffing increases.
Improved Compliance: HIPAA-compliant automation tools come with built-in safeguards and audit trails, offering a level of reliability that manual methods simply can't match.
These points make a strong case for transitioning to automated solutions.
Final Recommendation
Given the operational, financial, and compliance advantages outlined above, every U.S. clinic should assess its current workflows and prioritize EMR integration to stay competitive in today’s fast-evolving healthcare landscape.
Start by focusing on high-impact areas like document management or referral tracking. These processes often deliver quick wins, helping to build confidence in automation. Platforms like Diagna provide an excellent starting point with their seamless EMR compatibility and intuitive interface that requires minimal training.
It’s also crucial to choose solutions that align with your existing systems. Many successful implementations enhance workflows through targeted automation, while web-based platforms ensure accessibility for remote work scenarios.
Finally, track your progress. Measure metrics like processing times, error rates, and staff satisfaction to showcase tangible improvements and guide future investments in automation.
The evidence is undeniable: EMR integration outshines manual data entry in every category that matters. Clinics that delay this shift risk falling behind in an increasingly efficient and patient-focused industry. The time to make the move is now.
FAQs
×
How can a clinic start transitioning from manual data entry to EMR integration?
Transitioning from manual data entry to EMR integration requires thoughtful preparation and execution. Start by analyzing your clinic's current workflows to pinpoint areas where an EMR system could make a difference - like minimizing errors or streamlining time-consuming tasks. Once you've identified these needs, select an EMR platform that fits your clinic's priorities. Look for features like patient record management, appointment scheduling, and billing capabilities to ensure it covers all the essentials.
After choosing the system, create a detailed implementation plan. This should include staff training, transferring existing data, and running tests to confirm everything operates as expected. Introduce the system gradually by phasing out manual processes, giving your team time to adapt. To ensure long-term success, provide continuous support and resources to help your staff fully embrace the benefits of the new system.
×
How does EMR integration help meet HIPAA requirements compared to manual data entry?
EMR integration plays a key role in meeting HIPAA requirements by incorporating strong security features like encrypted data storage and restricted access. These measures protect sensitive patient information from unauthorized access and reduce the risks associated with manual data entry, which is often error-prone and less secure.
One standout feature of EMR systems is their ability to automate compliance tasks. They ensure that health data is managed securely and efficiently without relying on manual oversight. Beyond security, EMR systems maintain detailed logs of who accessed or modified data, offering a clear trail for tracking and audits. This level of oversight not only minimizes the chance of data breaches but also ensures daily operations align with HIPAA standards.
×
What challenges might clinics face when implementing EMR integration, and how can they address them?
Clinics often face hurdles like interoperability problems, where systems can't effectively share information due to mismatched data formats, and workflow disruptions, as existing routines may need to be restructured. There's also the challenge of user resistance, with staff sometimes reluctant to embrace new technology, and over-customization of EMR systems, which can make integration unnecessarily complex.
To tackle these issues, clinics can use standardized data exchange protocols and prioritize systems designed to communicate effortlessly. Choosing EMR solutions that are intuitive and compatible with current tools can simplify the process. Offering comprehensive training and consistent support helps staff adjust, paving the way for a smoother transition and long-term efficiency.